Digital pathology has been gaining momentum in recent years, and for good reason. Pathology labs worldwide are under growing pressure to deal with increasing workloads while maintaining quality standards. Pathologists are looking at technology to help them deal with these challenges.
In this article, we would like to address two important topics. First, we will describe the benefits of digital pathology. Second, we will discuss how to implement digital pathology and the importance of the pre-analytical aspects of sample processing in achieving this.
What is digital pathology?
Digital pathology refers to using a digital environment to acquire, manage, analyse, share and interpret pathology information. The essence of digital pathology is the whole slide image (WSI), a digital twin of the conventional tissue mounted and stained on a microscope glass slide. The WSI is obtained through a high-resolution scanner and viewed on a computer screen.
In the last decade, technological advances have facilitated the development of high-throughput pathology scanners capable of obtaining high-quality, clinical-grade images. That has made it possible for regulators to allow the use of these images for clinical use, resulting in the evolution and adoption of digital pathology for routine diagnosis.
This new technology attracts multiple benefits for pathologists and their patients, which explains the increasing interest in the field. However, its importance lies in the fact that it constitutes the foundation without which computational pathology – the use of artificial intelligence (AI) tools to aid diagnosis – wouldn’t be possible.
The benefits of digital and computational pathology
Early adopters of the new technology report significantly enhanced lab efficiency, which provides patients with faster, accurate diagnoses. However, there’s much more to it. Here are just a few digital pathology and AI benefits that make optimal patient care possible. As you’ll see, they are all interconnected, so digital pathology can be beneficial on multiple levels right from the start.
Greater diagnosis precision
Interpreting all the information present in a single tissue slide can be incredibly complex for pathologists. Tasks like biomarker quantification or accurate detection of small foci suspicious for cancer can be very challenging, mainly when pathologists are under pressure.
This is where AI can aid pathologists and help them achieve greater diagnostic precision. Naturally, this is incredibly important given the time constraints that pathologists are under.
Faster diagnoses
Aside from accuracy, another factor that digital pathology improves is turnaround time. This means a more efficient collaboration and faster diagnosis. For patients, this means less additional stress and uncertainty while waiting for results.
An impressive example is the Department of Clinical Genetics and Pathology, Region Skåne, a Swedish multisite laboratory that produces over 800,000 slides per year. When sharing his experiences with the implementation of digital pathology, Dr Kevin Sandeman, Clinical Pathologist and Head of Unit for pathology, stated that diagnosis and cancer care lead times had been greatly improved at the Department. To be precise, the total time to diagnosis has been reduced by 12.5%.
Lab workflow optimisation
Going digital has multiple advantages for histopathology labs. Preparing for tumour boards is more efficient and requires far less time. Archiving, organising, retrieving and sharing cases is faster.
This positively impacts the overall productivity of the lab and provides the workforce with more flexibility. A study from a Dutch pathology lab reported savings of 19 working hours per day in logistics, obtained across multiple professionals and different aspects of the workflow by going digital.

Pathologists’ reading times are shorter when digital pathology is implemented for routine diagnosis. This, coupled with the more efficient logistics across the lab, results in significant efficiency gains that can be as high as 20%, as reported by early digital pathology adopters.
Thus, by taking full advantage of the possibilities the digital environment presents, pathologists can provide accurate diagnoses to a larger number of patients within a shorter timeframe.
Improved collaboration
Digital pathology doesn’t enhance only the workflow within a single lab. Since cases and slides can be handled more efficiently, regardless of distance, digital pathology allows for cases to be assigned rationally across different labs that are geographically distant.
This, in turn, facilitates the creation of diagnostic networks in which pathologists can subspecialise in areas of diagnostic interest. This typically results in shorter turnaround times and greater diagnostic quality.
Consultation cases and collaboration across labs can be organised smoothly and without the hassle of complex logistics. This also facilitates education and collaborative assessments. By easing these processes, digital pathology advances diagnosis and makes it possible to cater to patients better.
Reduction of human error
Unfortunately, errors do happen in all areas of human endeavour, and pathology is no exception. To err is human at the end of the day, and although rare, diagnostic errors can have serious consequences. Thankfully, AI in pathology has demonstrated that it can help pathologists reduce diagnostic errors.
Small foci of tumour that can be easily missed during biopsy screening are easier to detect when AI highlights these problematic areas. In addition, when pathologists use AI, their reading times are shortened, thus not only becoming more efficient but also providing a better service for their patients.
Cost reduction
Thanks to the improved productivity achieved in fully digital pathology labs, the investment pays for itself in as little as 2-3 years, leading to a reduction in long-term costs. In addition, several studies are being performed on the long-term economic effects of improved accuracy thanks to AI aiding pathologists in their diagnoses.
Certainly, the easier collaboration and streamlined workflow due to digital pathology mean that there is less need for additional activities such as overtime and travel for case reviews, tumour boards, etc. Ultimately, this leads to more efficient time use across all pathology lab professionals.
How to fully leverage the power of digital pathology
Digital pathology may improve lab efficiency and patient care tremendously, but it’s not quite as simple to get there. Before reaching the digital phase, a lab must first thoroughly review the pre-analytical stage.
Optimising the pre-analytical phase facilitates the slide digitisation process and reduces scanning errors.
For this reason, labs aspiring to adopt digital pathology are recommended to finetune their pre-analytical process. This is to maximise the efficiencies realisable in a digital workflow can be materialised.
Therefore, proper slide preparation is key for a quality scanning result and accurate diagnosis. This is especially important with the integration of AI, since both algorithms and pathologists rely heavily on proper WSI quality to produce reliable diagnoses.
Sakura and digital pathology
Sakura’s primary role is to continuously provide innovations that make it possible to optimise the pre-analytical process and achieve the full potential of digital pathology. We aim to improve lab efficiency and advance cancer diagnosis through our standardisation and lab automation solutions, supporting maximum patient care.
Optimising the pre-analytical phase
Let’s take a closer look at the specific ways in which Sakura standardises each step of the pre-analytical process to facilitate digital pathology.
Grossing
At the grossing station, it is essential to ensure the tissue sections are of adequate size, thickness and present the correct cassette orientation. This has a knock-on effect on tissue processing, embedding and microtomy (more on this later).
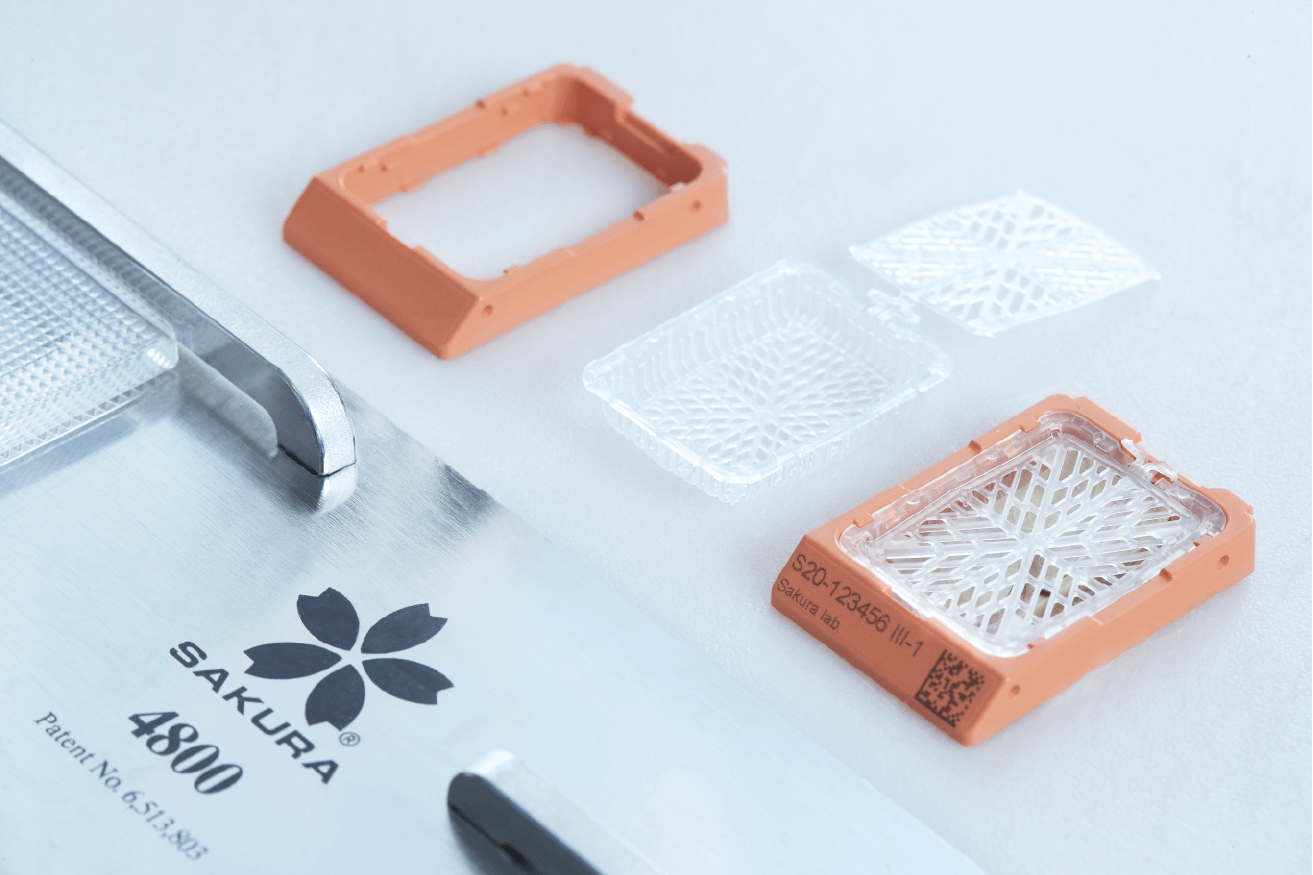
Sakura’s Tissue-Tek® Paraform® Sectionable Cassette System takes care of this. The Paraform cassette makes sure the tissue orientation remains correct throughout all the steps, so the risk of orientation errors is minimised.
Incorrect orientation may lead to a slide that may not reveal areas critical for diagnosis and may negatively affect the rest of the diagnostic process. Therefore, the grossing part of the workflow should be optimised for quality.
Tissue processing
In digital pathology labs, the scanning process can become one of the main bottlenecks for the entire workflow. This is so because scanners can only digitise one slide at a time. A solution to this challenge is to step away from the traditional batch approach and implement a continuous workflow in the lab.
In a traditional batch approach, conventional tissue processors require long turnaround times to produce a large batch of tissue cassettes that go on to the next steps on the workflow. During this time, the digital pathology scanners sit unused, waiting for these large batches of slides to arrive at the scanning step. And when they do, a bottleneck is created.
In a modern, continuous workflow lab, the tissue processors can generate smaller batches of tissue cassettes in a much shorter turnaround time continuously. Ultimately, it means scanners can ingest the workload created in a continuous fashion without creating bottlenecks.
The Tissue-Tek Xpress® x120 continuous rapid tissue processor kickstarts the continuous workflow in the lab, thus facilitating the maximised utilisation of scanners.
Tissue embedding
Tissue-Tek AutoTEC® a120, an automated embedder, carries on the continuous flow that the Tissue-Tek Xpress x120 started. This fully automated system embeds all blocks in a standardised way. And, since the tissue is embedded directly in the original Paraform cassette without requiring transfer to a paraffin mould, the chances of tissue being lost, misplaced, or wrongly reoriented are eliminated. This translates into greater efficiency and patient safety.
Microtomy
Tissue thickness has an important effect on digital WSIs. The cellular overlapping may hinder the assessment of these thicker sections.
The tissue section thickness is also important to aid the autofocus mechanism of digital pathology scanners. Sakura’s Tissue-Tek AutoSection® makes it possible to cut sections of a consistent thickness and standardise your microtomy as preparation for digital pathology.
Staining and coverslipping
Since digital pathology scanners require adequate contrast to detect tissue areas and to obtain sharp focus images, it is essential that low contrast tissue is optimally stained. This way, the digital image obtained is a faithful replica of the original.
Sakura has developed the H&E Staining Kit to minimise staining variations. Together with the recommended Sakura® H&E protocol for the Prisma Plus, it minimises process variation and gives clear, quickly stained slides to facilitate accurate diagnostics.

Another crucial factor is coverslipping. Air bubbles, dust and excess mounting media are common causes of scanning errors. Sakura’s automated Tissue-Tek Film® Coverslipper reduces these troublesome artefacts that could affect the image quality as well as the scanning process. Slides oozing excess mounting media can be a major headache for digital pathology labs.
'Complete Digital Pathology for Routine Histopathology Diagnosis in a Multicenter Hospital Network' describes the methodology and resulting experience at the Granada University Hospital in Spain. This pathology lab has successfully transitioned to an entirely digital way of working. Since 2016, they have been a fully operational digital laboratory for primary histopathology. The paper also highlights that the film coverslipper has made it possible to minimise errors by eliminating mounting media-oozing slides that “interfere with the mechanical elements of the scanning system” (Retamero et al., 2020), a well-known source of scanning errors. And in addition, scanning is 3.7% faster on coverslipping film than glass.
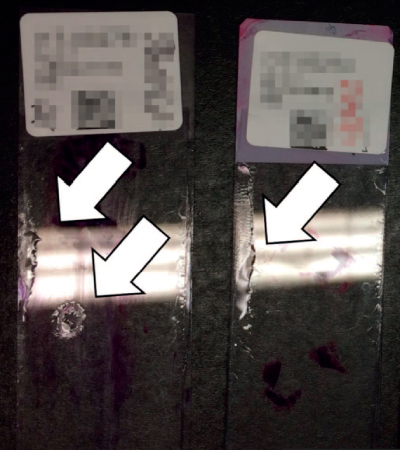2.png)
Challenges faced
During the test phase toward a full digital workflow 11,758 glass slides including H&E, histochemistry and immunochemistry were scanned revealing the following errors:
- The most common error encountered was the number of slides being skipped due to an unrecognisable QR code. This can result from poor slide label quality or pigment splatters on the label during the staining.
- Another common error happens when the scanner’s robotic arm prongs and the stage mechanisms malfunction, resulting in the digitised slide not being released properly. The cause can either be due to a label misalignment and sticking to the prongs, or an excess in mounting media in a slide.
- In the case of excess mounting media on a slide, the mounting media will interfere with the scanner’s optical system and will require a full clean-up.
Overcoming the challenges
The above challenges greatly impact the digital workflow and the quality of the digitised slide images. In order to overcome them, one needs to ensure that:
- Glass slides are clean and free of artefacts that may unnecessarily increase the scanning time.
- The histological preparations have carefully placed coverslips that are well aligned.
- The histological preparations have slides that are free from excess mounting media that would otherwise interfere with the mechanical elements of the scanning system.
With staining and coverslipping being such crucial steps towards a superior digital slide, Sakura has developed an integrated system, Tissue-Tek Prisma® and Tissue-Tek Film®, to foster standardisation further and facilitate the transition to digital pathology. The article discussed above states that since the adoption of Sakura’s Tissue-Tek Coverslipping Film, scanning errors have been minimised. The Tissue-Tek Coverslipping Film is the 5th generation resin-coated plastic film that eliminates the need for cover glass and liquid mounting medium. It reduces coverslipper maintenance and enables fast coverslipping. Sakura Finetek is the innovator and industry leader in providing this product for over 30 years.
The Tissue Tek Coverslipping Film provides the following benefits:
- Fewer air bubbles compared with glass coverslips.
- Film coverslipping is faster compared with glass coverslipping.
- The Film coverslipped slides dry quicker than glass coverslipped slides, and can therefore be placed in the scanner sooner.
- Minimising errors for digital pathology as it is free from excess mounting media and leaves almost no residue.
- There is no risk of glass coverslips breaking that could disrupt the scanning process.
Conclusion
There’s no doubt that pathology is at an inflexion point towards a revolution in the field of tissue diagnostics. The boost in lab workflow and efficiency certainly enables faster and better diagnoses for patients. It also prepares both the area and pathologists themselves for the more advanced computational pathology. Optimisation of the pre-analytical phase facilitates a lab in switching to digital pathology.





